What is Precision Emergency Medicine?
Precision emergency medicine is the use of information and technology to effectively, efficiently, and authentically deliver acute care for individual patients and their communities.
Precision emergency medicine includes the adoption of a range of patient-centered processes and targeted health outcomes. These practices evolve in response to technological advancements, changes in individual or population health data, and consumer demand.
How does precision emergency medicine impact clinical practice?
Precision emergency medicine aims to help providers and systems become even more patient-centered. Through precision emergency medicine, we can better interpret data about our patients, helping us refine and tailor individualized clinical care.
How does precision emergency medicine improve care?
Adopted correctly, precision emergency medicine can ensure seamless and accelerated access across healthcare settings, increased personalization of diagnostics and therapeutics, improved short and long-term health outcomes, and an increased ability for patients to make informed and authentic healthcare decisions.
Why is emergency medicine a key driver of precision health care?
Emergency physicians are uniquely suited to a broad adoption of precision health, given our understanding of the social determinants of health and the challenges of inconsistent access to care.
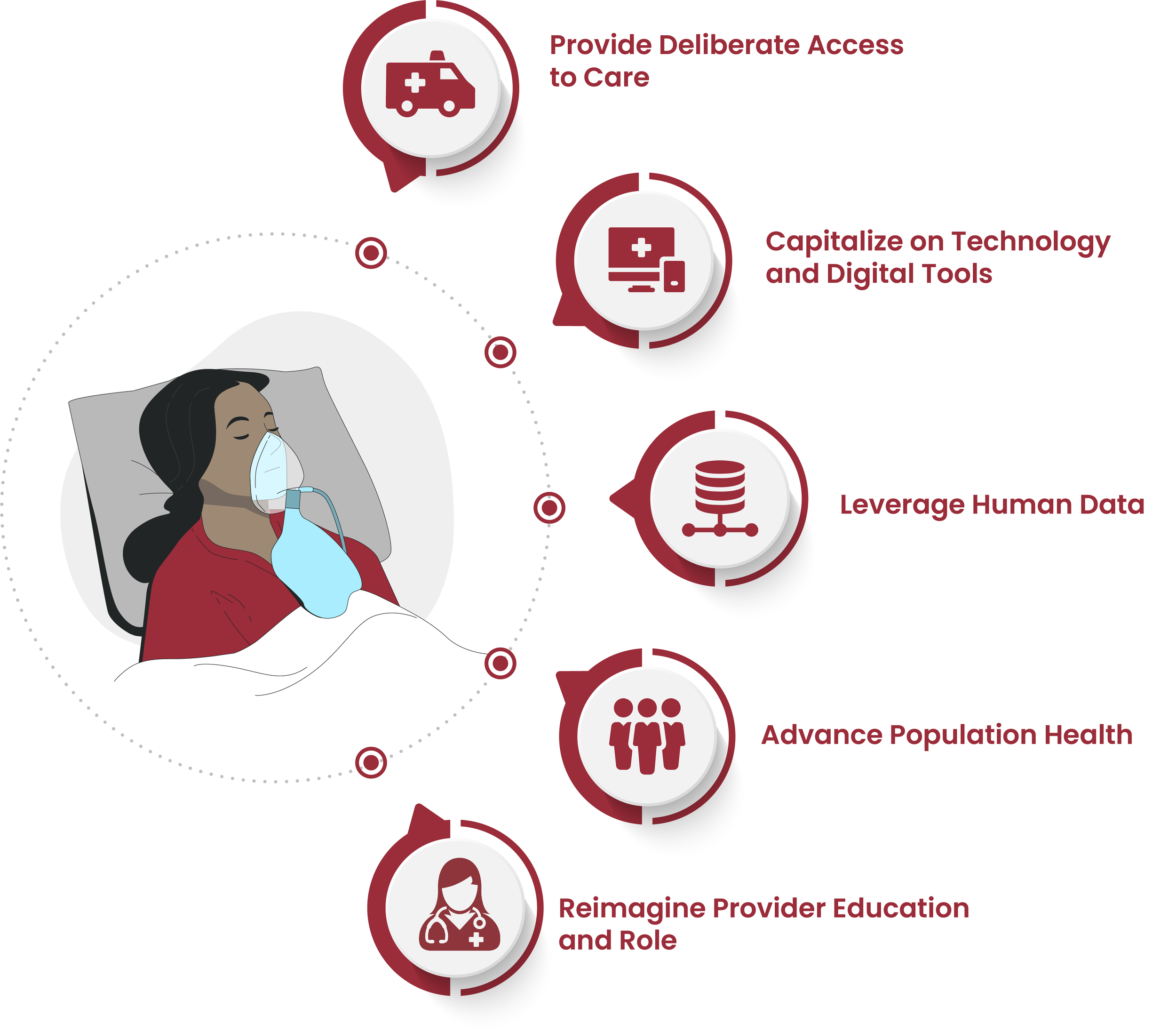
Precision emergency medicine includes the adoption of a range of patient-centered processes and targeted health outcomes in five key areas.
Provide deliberate access to care
Expand telehealth access
Optimize clinical care location
Strengthen linkages to post-acute care
In a precision emergency medicine system, access to care is individualized to patients based on their specific needs and information in their health record.
The right location for treatment varies by illness severity and may be dynamic as diseases progress.
The patient and their data are the hub of precision emergency medicine, with the physical emergency department being just one of many avenues available to address acute patient needs.
Capitalize on technology and digital tools
Incorporate new data sources
Accelerate use of novel diagnostics
Individualize treatments
Rapid advances in technology leading to incremental improvement in the accuracy and timeliness of diagnostic testing -- with near-immediate results for biomarkers and imaging -- have fundamentally changed emergency care over the past few decades.
Precision emergency medicine is fueled by continued advancements in data acquisition that empower physicians to further individualize the care of undifferentiated patients.
Leverage human data
Integrate data science and AI
Merge advances in informatics
Create a learning health system
Incorporate social determinants of health
Human data are sourced, reconstructed, and integrated in ways never before imagined. Billions of data points are used to construct detailed portraits of patients.
Utilizing machine learning, these in-depth profiles are compared to individuals with similar socio-behavioral phenotypes, as well as population data, to make ever more accurate diagnoses and outcomes predictions.
Advance population health
Strengthen disease tracking and treatment
Inform community and public health agencies
Prioritize population health initiatives
Precision emergency medicine recognizes that social and environmental factors play a central role in health.
Emergency departments can be key contributors to population health surveillance through the deliberate collection of data.
Data is used to create social phenotypes that, when combined with individual patient information, better predict risks, outcomes, and the design of successful interventions.
Strategic partnerships with the larger public health system offer great potential for disease detection, tracking, and interventions that are only now being explored.
Reimagine provider education and role
Use and interpret data accurately
Share decision-making with informed patients
Achieve competence in health data literacy
Widespread adoption of precision emergency medicine will require that we educate providers to use data and technology differently to enhance patient care. Physician education in health data literacy, digital health, and implementation science is imperative, especially given the wide variability in physicians’ knowledge and experiences in these domains. Expertise in these areas will be achieved only through a fundamental evolution of medical education based on this new conceptual model.